Imagine a world without thermometers. A world where a simple, physical sign like fever, a fundamental indicator of illness, remains a mystery. While we might not be living in that world, it’s not too long ago that the complexities of fever were shrouded in ambiguity. Today, thanks to dedicated medical professionals and a growing understanding of human physiology, we can identify not only the presence of fever but also its underlying causes. Nursing, with its meticulous attention to detail and holistic approach to patient care, plays a crucial role in deciphering the puzzle of fever, unraveling the “why” behind the “what.”
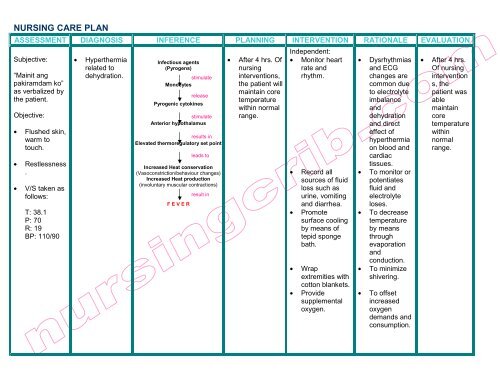
Image: www.yumpu.com
Fever, technically known as hyperthermia, is a complex physiological response to an invading pathogen or internal stressor. It is not a disease itself but a symptom often indicative of a broader health concern. Nursing diagnosis, therefore, involves more than just observing the fever; it necessitates understanding the unique context of each patient, carefully analyzing their individual history, symptoms, and potential risk factors. This article will explore the intricate world of nursing diagnosis for patients experiencing fever, examining the key considerations, common nursing diagnoses, and actionable interventions that contribute to effective and compassionate care.
Understanding the Fever: A Multifaceted Approach
Fever is a key indicator, a red flag waving for the vigilant nurse. But understanding it is not as simple as just taking a temperature reading. It’s about digging deeper, piecing together a story told through various symptoms, patient history, and physical observations.
1. The Vital Sign: Temperature
The cornerstone of fever diagnosis is temperature measurement. Nurses use various thermometers—oral, rectal, axillary, or temporal—to obtain precise readings. Understanding normal temperature ranges for different age groups and methods is essential. For instance, a rectal temperature reading is typically considered more accurate than an oral reading, especially in infants and young children. The fever itself provides important clues: is it mild, moderate, or high? Is it persistent or intermittent? The fever’s nature tells a story.
2. Beyond the Thermometer: The “Why” Behind the Fever
Fever is not a stand-alone phenomenon. It is often accompanied by other symptoms, each offering valuable insights. These may include:
- Sweating: Fever often triggers sweating as the body attempts to regulate temperature. Excessive sweating, especially when accompanied by fever, could indicate a severe infection.
- Chills: The body shivers involuntarily to generate heat, resulting in chills. This often precedes a fever spike.
- Headache: A throbbing headache is a common complaint, particularly with fevers related to viral or bacterial infections.
- Muscle aches: This is a characteristic symptom associated with fever, especially with viral infections like influenza.
- Loss of appetite and fatigue: A weakened immune system and the body’s focus on fighting off infection often lead to decreased appetite and general fatigue.
- Rapid breathing: An elevated respiratory rate, known as tachypnea, can be a sign of fever’s impact on the body’s oxygen demand.
- Rapid heart rate: Increased heart rate, also called tachycardia, can be attributed to the body’s efforts to maintain blood flow and oxygen supply during fever.

Image: nurseslabs.com
3. The Patient’s Story: Past Medical History & Risk Factors
Every patient is unique, with their own medical history and risk factors contributing to their overall health. A thorough assessment of the patient’s past medical history is crucial. For instance, a patient with a known history of autoimmune disorders might be more susceptible to infections leading to fever, or a patient receiving chemotherapy might be at higher risk of developing febrile neutropenia, a serious condition characterized by fever and low white blood cell count.
4. The Power of Observation: Physical Assessment
Physical examination is a powerful tool in the nurse’s arsenal. Observations like skin condition (flushed, pale, or mottled), lymph node swelling, respiratory sounds, and signs of dehydration all contribute to a comprehensive picture.
Common Nursing Diagnoses for Patients with Fever
Based on the collected data from temperature readings, symptom analysis, and patient history, nurses can formulate nursing diagnoses. These diagnoses pinpoint the underlying problems, guiding the development of targeted interventions. Below are some common nursing diagnoses associated with fever:
1. Hyperthermia:
This is a direct response to the elevated temperature. Nurses implement interventions to reduce fever, such as cooling measures, promoting fluid intake, and administering antipyretic medications.
2. Risk for Ineffective Thermoregulation:
This diagnosis applies when factors like age, medication use, or underlying conditions increase the risk of the patient’s body struggling to regulate temperature effectively. Interventions focus on monitoring temperature closely and ensuring the patient’s environment is conducive to maintaining a stable temperature.
3. Risk for Infection:
This is particularly relevant when the fever is a potential sign of a lurking infection. Nurses prioritize infection control measures like hand hygiene, proper wound care, and appropriate isolation protocols when indicated.
4. Acute Pain:
Fever can cause discomfort and pain, particularly headaches and muscle aches. Nurses aim to manage pain through non-pharmacological interventions like positioning, massage, and distraction techniques, as well as appropriate analgesics if needed.
5. Fluid Volume Deficit:
Fever can lead to increased fluid loss through sweating and increased respiratory rate. Nurses monitor hydration status closely, encouraging fluid intake and addressing any signs of dehydration.
Nursing Interventions: A Framework for Care
The nursing diagnosis guides interventions designed to alleviate symptoms, address underlying causes, and promote overall patient well-being. These interventions may include:
1. Fever Reduction:
This is a primary goal for many patients with fever. Nurses employ various methods, such as:
- Cooling measures: Applying cool compresses, bathing with tepid water, and using fans for air circulation can help lower body temperature.
- Promoting fluid intake: This helps replace fluids lost through sweating and maintain hydration.
- Administering antipyretics: Medications like acetaminophen or ibuprofen can effectively lower fever.
2. Infection Control:
When infection is suspected, nurses implement strict infection control measures to prevent further transmission. This may involve:
- Hand hygiene: Frequent handwashing with soap and water or using alcohol-based hand rubs is essential.
- Isolation protocols: Using contact precautions or droplet precautions as indicated to minimize the spread of pathogens.
- Wound care: Careful management of wounds to prevent infection.
- Collecting specimens: Obtaining blood cultures, urine samples, or other specimens for laboratory analysis to identify the causative organism.
3. Pain Management:
Nurses provide comfort and relief from fever-related pain through:
- Non-pharmacological interventions: Positioning, massage, relaxation techniques, and distraction methods can help.
- Analgesics: Administration of over-the-counter or prescription pain relievers as needed.
4. Hydration Support:
Nurses ensure adequate hydration by:
- Monitoring intake and output: Tracking the patient’s fluid intake and urine output to assess hydration levels.
- Encouraging oral fluids: Offering frequent sips of water, juice, or clear broth while avoiding sugary drinks.
- Intravenous fluids: Administering intravenous fluids if oral intake is inadequate.
5. Patient Education:
Nurses empower patients to participate in their care by:
- Explaining the cause of fever: Providing clear and understandable information about the potential causes of fever.
- Teaching fever management techniques: Instructing patients on home care measures such as taking medications, using cooling techniques, and monitoring their temperature.
- Emphasizing the importance of follow-up: Ensuring patients understand when they should seek medical attention for fever and follow up with their physician.
Nursing Diagnosis For Patient With Fever
Conclusion: The Art and Science of Nursing Care
Nursing diagnosis for patients with fever is about much more than simply recording a temperature. It’s about a holistic, personalized approach that combines the art of observation and the science of clinical knowledge. Nurses, through their keen assessment, compassionate care, and tailored interventions, play a vital role in not just treating fever but uncovering the underlying reasons for it. They are the guardians of the patient’s health, weaving a tapestry of medical knowledge, clinical expertise, and empathy to offer patients the best possible care. By understanding the complex world of fever, we strengthen the connection between symptom and root cause, ultimately empowering patients to regain their health and well-being.






