The rhythmic thump of a heart is the symphony of life, a vital organ working tirelessly to pump blood throughout our bodies. But what happens when this symphony falters, when the very lifeline that sustains us is threatened by a silent, insidious enemy – ischemic heart disease? This condition, characterized by reduced blood flow to the heart, affects millions worldwide, often leaving patients and their families grappling with uncertainty and fear. This article delves into the world of ischemic heart disease, shedding light on its complexities and exploring the vital role of nursing care in managing this chronic and potentially life-threatening condition.
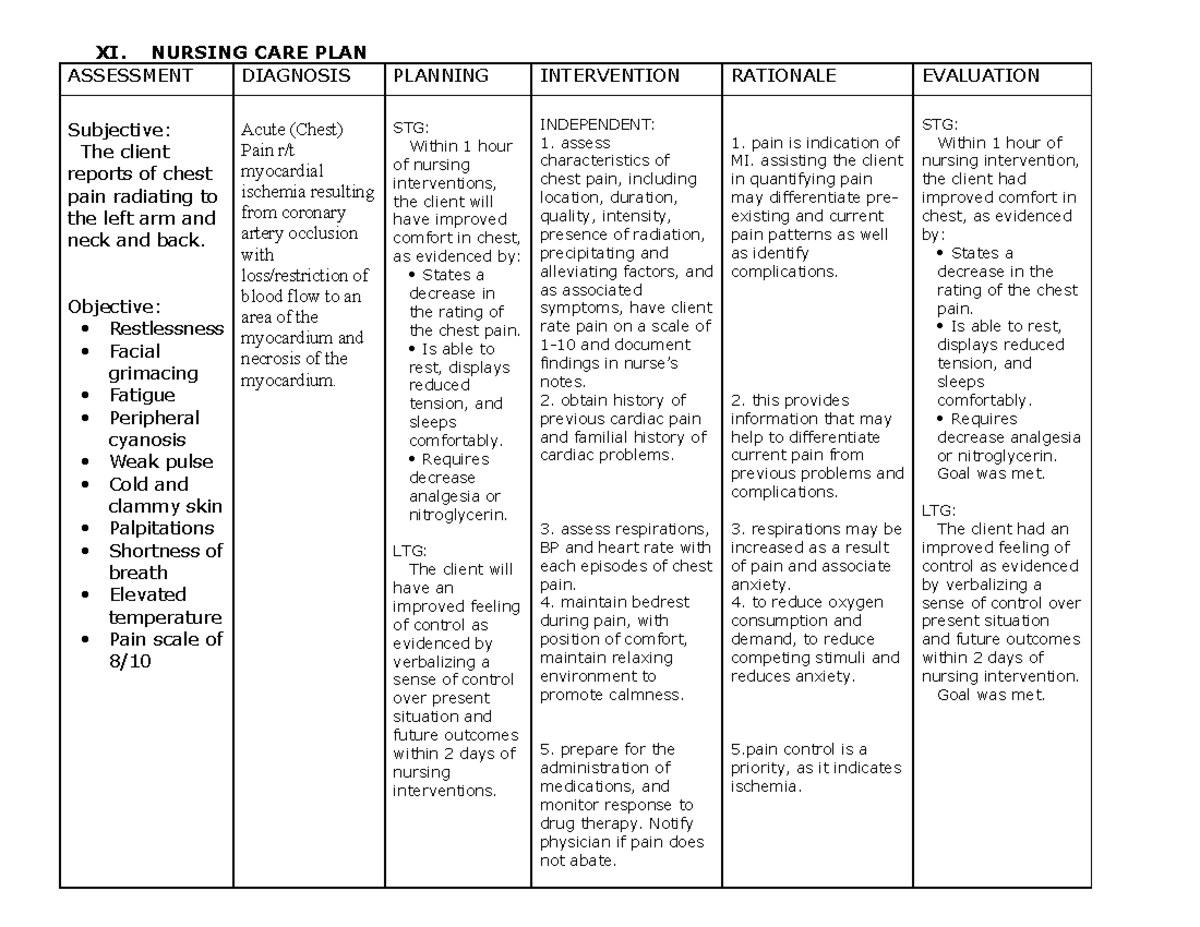
Image: www.studocu.com
I remember a patient, Mrs. Johnson, who arrived at the cardiac ward with a look of sheer terror in her eyes. As a nurse, I knew the diagnosis of ischemic heart disease was a heavy burden, but seeing the fear in her eyes made me realize the profound impact it has on individuals and their loved ones. Mrs. Johnson’s story, like many others, underlined the importance of comprehensive nursing care in supporting patients with ischemic heart disease. The journey to recovery is long and demanding, requiring not only medical expertise but also compassionate and empathetic nursing care to navigate the challenges and empower patients to manage their condition actively.
Understanding Ischemic Heart Disease
Ischemic heart disease, often referred to as coronary artery disease (CAD), arises from the narrowing or blockage of coronary arteries – the blood vessels that provide oxygen and nutrients to the heart. This narrowing, typically due to atherosclerosis (the buildup of plaque), restricts blood flow, leading to chest pain (angina), shortness of breath, and in severe cases, a heart attack. The consequences of ischemic heart disease can be devastating, ranging from debilitating symptoms to life-threatening events.
The impact of ischemic heart disease transcends individual health, affecting families and communities. It is a leading cause of death globally, underscoring the critical need for effective prevention, early detection, and comprehensive management strategies. This is where the role of nursing care comes into play, creating a crucial bridge between medical interventions and the patient’s overall well-being.
A Comprehensive Nursing Care Plan: A Roadmap to Recovery
Developing a comprehensive nursing care plan for patients with ischemic heart disease requires a multi-faceted approach that addresses the unique needs of each individual. The plan should be tailored to the patient’s specific condition, risk factors, and overall health status. It is crucial to understand that ischemic heart disease is a chronic condition requiring ongoing management, prevention, and support. The aim is to empower patients to take an active role in their health and achieve optimal quality of life.
Assessment and Monitoring
The foundation of a successful nursing care plan lies in a thorough assessment, including a comprehensive health history, physical examination, and diagnostic tests. This allows nurses to gain a clear understanding of the patient’s symptoms, risk factors, and the progression of the disease. Regular monitoring is equally critical, assessing vital signs, cardiac rhythms, and pain levels. Nurses play a vital role in identifying early changes in the patient’s condition that may signal complications, enabling prompt intervention and minimizing potential risks.

Image: www.myxxgirl.com
Education and Support
Empowering patients with knowledge is key to promoting self-management and adherence to treatment plans. Nurses provide education about their condition, medications, lifestyle changes, and risk reduction strategies. They explain the importance of regular check-ups, stress management techniques, and healthy lifestyle choices. Compassionate support is equally vital, providing patients with a safe space to express concerns, ask questions, and cope with the emotional and psychological impact of the condition.
Medication Management
Patients with ischemic heart disease often require a combination of medications to manage their condition. Nurses play a crucial role in ensuring that patients understand their medications, their potential side effects, and the importance of adhering to the prescribed dosage and schedule. They also monitor for any adverse drug reactions and work collaboratively with physicians to adjust medications as needed. This comprehensive approach to medication management ensures optimal therapeutic outcomes while minimizing potential complications.
Lifestyle Modification
Lifestyle modification is an essential component of ischemic heart disease management. Nurses advise patients on adopting healthy habits, including regular physical activity, maintaining a healthy weight, quitting smoking, and managing stress. They provide guidance on making dietary changes, such as reducing saturated and trans fats and incorporating fruits, vegetables, and whole grains into their diet. Tailoring these recommendations to individual preferences and needs promotes long-term adherence and positive outcomes.
Emotional and Psychological Support
The diagnosis of ischemic heart disease can be emotionally overwhelming, creating anxiety, fear, and uncertainty. Nurses provide emotional support, listening attentively to patients’ concerns and offering a compassionate presence. They guide patients towards coping mechanisms, such as relaxation techniques, counseling, or support groups, helping them manage stress and build resilience. This holistic approach to care addresses the emotional and psychological needs of patients, fostering a sense of hope and empowering them to navigate their journey with greater strength.
Latest Trends and Developments
The field of cardiovascular care is constantly evolving, with new research findings and technological advancements shaping the landscape of ischemic heart disease management. The advent of minimally invasive cardiac procedures, such as stent placement and coronary artery bypass surgery, has revolutionized treatment options, offering less invasive and more effective solutions for patients. Advancements in diagnostic imaging, such as coronary computed tomography angiography (CCTA), allow for earlier detection and better risk stratification, enabling targeted interventions and improved outcomes.
Furthermore, the emphasis on personalized medicine and precision cardiac care is gaining traction. This approach aims to tailor treatment strategies based on an individual’s genetic makeup, lifestyle factors, and other patient-specific characteristics. By understanding the unique biological factors influencing the progression of ischemic heart disease, healthcare professionals can develop more effective and personalized treatment plans. These developments hold immense promise for enhancing patient care and improving long-term outcomes.
Expert Tips for Nursing Care
My experience as a nurse has taught me that effective nursing care requires a blend of technical skills, empathy, and a genuine desire to help patients navigate their challenges. Here are a few key tips that I have found invaluable in providing optimal care to patients with ischemic heart disease:
1. **Build Strong Patient Relationships:** Establishing trust and rapport is paramount. Take the time to listen to patients’ concerns, answer their questions, and provide clear explanations about their condition and treatment plan. Open communication fosters a sense of partnership, empowering patients to actively engage in their care.
-
Focus on Patient Education: Emphasize the importance of lifestyle modifications and adherence to medication regimens. Provide patients with educational materials tailored to their needs and demonstrate practical strategies for managing their condition. Empowering patients with knowledge enhances their understanding, promotes self-management, and improves outcomes.
-
Promote Physical Activity: Encourage patients to engage in regular physical activity within their limitations. Provide guidance on safe and effective exercise programs that align with their condition and overall health status. Physical activity not only improves cardiovascular health but also reduces stress, elevates mood, and enhances overall well-being.
-
Encourage Stress Management: Address the psychological impact of ischemic heart disease by promoting stress management techniques. Guide patients towards relaxation methods, such as deep breathing exercises, meditation, or yoga, to manage stress levels and improve their mental and emotional health.
-
Facilitate Social Support: Recognize the importance of social connections and support systems. Encourage patients to engage in support groups or connect with others who have similar experiences. Social support networks can provide valuable emotional support, motivation, and a sense of community, enhancing their overall well-being and coping skills.
Frequently Asked Questions
Q: What are the common symptoms of ischemic heart disease?
A: Chest pain or discomfort (angina), shortness of breath, fatigue, nausea, sweating, and lightheadedness are common symptoms. However, it is important to note that these symptoms can vary from person to person and may not always be present.
Q: What are the risk factors for ischemic heart disease?
A: Risk factors include high blood pressure, high cholesterol, smoking, diabetes, obesity, lack of physical activity, family history of heart disease, and age.
Q: How can I prevent ischemic heart disease?
A: Maintaining a healthy lifestyle through regular exercise, a balanced diet, managing stress, and avoiding smoking are crucial preventative measures.
Q: What are the treatment options for ischemic heart disease?
A: Treatment options may include medications, lifestyle modifications, minimally invasive procedures (e.g., stenting), and open-heart surgery. The specific treatment plan will depend on the severity of the condition and the individual’s overall health status.
Q: What are the long-term implications of ischemic heart disease?
A: Ischemic heart disease is a chronic condition that requires ongoing management and risk reduction strategies. Following a healthy lifestyle, regularly monitoring your condition, and maintaining close communication with your healthcare team are essential for optimizing long-term well-being.
Ischemic Heart Disease Nursing Care Plan
Conclusion
Providing comprehensive nursing care for patients with ischemic heart disease is a crucial aspect of managing this chronic and potentially life-threatening condition. This article has explored the complexities of this disease, emphasizing the importance of assessment, monitoring, education, support, and lifestyle modifications. We have also highlighted the latest trends and advancements in cardiac care, emphasizing the importance of personalized medicine and precision cardiac care. By embracing these principles and implementing a comprehensive nursing care plan, we can empower patients to take control of their healthcare, manage their condition effectively, and improve their quality of life.
Are you interested in learning more about ischemic heart disease and the role of nursing care in its management? Please share your thoughts and questions in the comments below. Let’s continue to promote awareness, understanding, and effective care for individuals facing this challenging health condition.






