Imagine you’re a nurse caring for a patient who can’t eat normally. Maybe they’ve had surgery, or they’re battling a disease that makes swallowing difficult. They need nourishment, but their bodies can’t take it in the usual way. What do you do? This is where the “enteral feeding” comes in. Enteral feeding is a life-saving technique that delivers nutrients directly into the stomach or small intestine, bypassing the mouth. But it’s not a simple process. It requires careful planning and constant monitoring. This is where the nursing care plan for enteral feeding comes in. This plan acts as a roadmap, guiding nurses through the complexities of ensuring patients receive the vital nourishment they need.

Image: heilienconley.blogspot.com
Enteral feeding can be a lifesaver, but it’s not without its challenges. Nurses are the frontlines of this battle, ensuring their patients receive accurate dosages, appropriate formulas, and continuous monitoring. They play a critical role in minimizing the risk of complications and maximizing the benefits of enteral nutrition. A well-structured nursing care plan for enteral feeding is the key to success in this vital area of care.
Understanding the Foundation: A Deep Dive into Enteral Feeding
Enteral feeding is a critical aspect of healthcare that involves providing nourishment directly into the gastrointestinal tract, bypassing the mouth and normal swallowing process. This method is used for patients who are unable to consume adequate nutrition orally due to various medical conditions. Its effectiveness hinges on a deep understanding of the feeding process and its potential complications.
The Roots of Enteral Feeding
The concept of enteral feeding has its roots in ancient medical practices. The earliest civilizations recognized the need to provide nourishment to those who were unable to eat normally. For instance, early cultures used tubes and devices akin to feeding tubes to deliver nourishment to patients with swallowing difficulties. However, it’s the advancements in medical technology and understanding in the 20th century that have revolutionized enteral feeding. With the development of more sophisticated feeding tubes and formulas, enteral feeding has become a vital tool in modern medicine.
Defining the Purpose
Enteral feeding has a singular purpose: to meet the patient’s nutritional needs. This vital nutritional support helps maintain healthy weight, promotes tissue repair and healing, and provides essential energy for the body. But it’s not just about physical sustenance; it’s also about enhancing their quality of life. Proper nutrition can help improve a patient’s ability to participate in daily activities and contribute to their overall well-being.
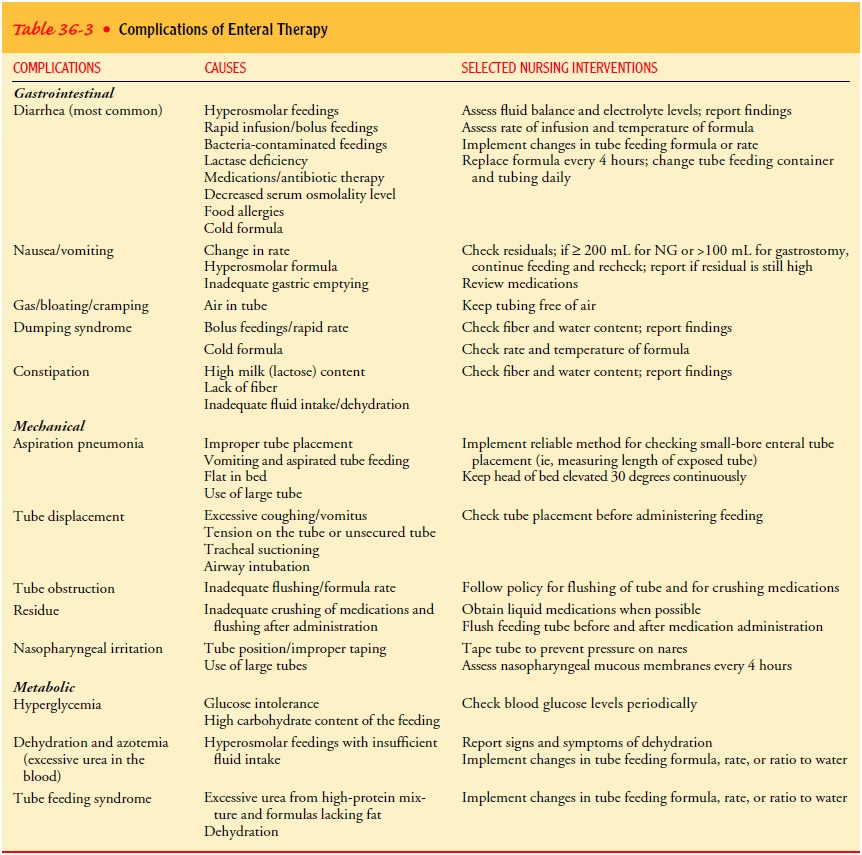
Image: www.vrogue.co
Types of Enteral Feeding
Enteral feeding can be accomplished using various methods and modalities. The choice of method depends on the individual patient’s needs and their ability to tolerate feeding. Some common types of enteral feeding include:
- Nasogastric (NG) Feeding: This is the most common method, involving inserting a thin tube through the nostril, down the esophagus, and into the stomach. NG tubes are useful for short-term feeding and are often used for patients who require immediate nutritional support.
- Orogastric (OG) Feeding: This method is similar to NG feeding, with the only difference being the insertion point through the mouth instead of the nose.
- Nasoduodenal (ND) Feeding: This method utilizes a longer tube inserted through the nostril, reaching past the stomach and into the duodenum. It is often used for patients with delayed gastric emptying or those at risk for aspiration.
- Nasojejunal (NJ) Feeding: This method involves a tube inserted through the nostril and placed into the jejunum, a section of the small intestine. It is a common choice for patients who have a high risk of aspiration or who are unable to tolerate feeding into the stomach.
- Gastrostomy (G-tube): A gastrostomy tube is placed surgically directly into the stomach. G-tubes are used for patients requiring long-term enteral feeding and are a safe and effective way to provide nourishment.
- Jejunostomy (J-tube): A jejunostomy tube is placed surgically directly into the jejunum. J-tubes are usually used in situations where there is blockage or issues with the stomach, making feeding through the stomach unsafe or ineffective.
Formulas – Fueling the Body
Enteral feeding formulas are carefully crafted mixtures of nutrients tailored to meet the patient’s specific needs, and the selection is crucial for optimal outcomes. There are various formulas available, which can be categorized according to their nutritional density, calorie content, and specific needs.
- Standard Formulas: These formulas are routinely used for patients with moderate nutritional needs and are often a good starting point. They typically contain a balanced mix of protein, carbohydrates, and fats.
- High-Calorie Formulas: These formulas are designed for patients who need more calories due to increased energy expenditure or malabsorption.
- High-Protein Formulas: These formulas are appropriate for patients experiencing protein loss due to illness or injury.
- Specialty Formulas: These formulas are tailored to address specific medical conditions. For example, renal formulas are designed for patients with kidney disease, while diabetic formulas are developed for patients with diabetes.
Challenges and Complications
Enteral feeding is not without its risks and challenges. Nurses must be aware of these potential problems and take proactive steps to mitigate them. Common complications include:
- Aspiration: This occurs when formula flows into the lungs, posing a significant risk of pneumonia.
- Diarrhea: This can be caused by the formula, medications, or changes in the gut flora.
- Constipation: This can result from the formula’s composition or decreased mobility.
- Dehydration: Inadequate fluid intake can exacerbate dehydration in patients receiving enteral feeding.
- Electrolyte Imbalances: Enteral formulas can sometimes contribute to electrolyte imbalances, requiring careful monitoring and adjustments.
Role of the Nurse: Navigating the Complexity
The role of the nurse is crucial in the success of enteral feeding. Nurses are responsible for:
- Assessment: Nurses gather information about the patient’s nutritional status, medical history, and any potential risks.
- Planning: Nurses develop a detailed care plan that addresses the patient’s specific needs, including the type of feeding tube, formula, and schedule.
- Implementation: Nurses manage the feeding process, ensuring the formula is delivered correctly and safely. They also monitor the patient for any signs of complications.
- Evaluation: Nurses continually assess the effectiveness of the feeding plan and adjust it as necessary. They document the patient’s response and any changes in their condition.
Essential Elements of a Comprehensive Nursing Care Plan
A well-structured nursing care plan for enteral feeding is paramount to providing safe and effective nutritional support. This plan outlines the specific actions and interventions nurses must undertake to meet the patient’s needs. Here are the essential elements:
- Patient Assessment: The nursing care plan begins with a thorough assessment of the patient’s nutritional status, allergies, medical history, and any potential risks.
- Feeding Tube Selection: The choice of feeding tube depends on the patient’s condition and the duration of feeding. The nurse should consider the patient’s anatomy, the feeding schedule, and potential risks of aspiration.
- Formula Selection: Appropriate formula selection is critical for meeting the patient’s nutritional needs. The nurse should choose a formula based on the patient’s age, medical condition, and calorie requirements.
- Feeding Schedule and Rate: The feeding schedule and rate must be tailored to the patient’s individual needs and tolerance level. Nurses should consider the patient’s digestive capacity, fluid needs, and potential for complications.
- Monitoring for Complications: Close monitoring is essential to identify and manage potential complications. Nurses must pay attention to the patient’s vitals, weight, bowel movements, and any signs of aspiration, gastrointestinal distress, or dehydration.
- Patient Education: The nurse educates the patient and family about enteral feeding, providing clear explanations of the process, potential complications, and home care instructions.
- Documentation: Comprehensive documentation is crucial for accurate record-keeping. The nurse should document the feeding plan, any changes in the plan, the patient’s response to feeding, and any adverse events.
Navigating Challenges: Expert Insights and Actionable Tips
Enteral feeding can be a complex and challenging process. But by understanding the core principles and practical tips, nurses can provide optimal care to their patients.
- Aspiration Prevention: Elevate the head of the bed to at least 30 degrees during and after feeding to minimize the risk of aspiration.
- Formula Integrity: Ensure that formula is prepared correctly and stored properly. Use sterile technique when preparing and administering the formula.
- Tube Placement Confirmation: Always verify the correct placement of the feeding tube before administering the formula. This can be done through aspiration or X-ray confirmation.
- Monitoring for Complications: Be vigilant in monitoring the patient for signs and symptoms of complications, such as aspiration, diarrhea, constipation, dehydration, or electrolyte imbalances.
- Patient and Family Education: Provide comprehensive education to both the patient and family about enteral feeding, the importance of medication management, and early recognition of any problems with the feeding.
Nursing Care Plan For Enteral Feeding
Conclusion: Empowering Effective Enteral Feeding Care
Navigating the landscape of enteral feeding requires a comprehensive understanding of the process, the potential for complications, and the role of the nurse as a key player in ensuring patient safety and well-being. A well-structured nursing care plan for enteral feeding is the cornerstone of providing optimal nutrition for patients who cannot eat normally. This plan acts as a guide, outlining the essential steps nurses must take to meet the individual needs of their patients. By adhering to these practices and remaining vigilant in monitoring their patients, nurses can empower patients to achieve a better quality of life through the vital support of enteral feeding.
This article is intended as educational material and should not be considered as medical advice. For specific medical information, consult with a qualified healthcare professional. If you are considering using enteral feeding for yourself or a loved one, it is essential to consult with a doctor or registered dietitian to ensure that it is the right option and to develop a personalized plan tailored to your needs.






