Imagine this: you wake up feeling a familiar pang of discomfort in your abdomen. The bathroom becomes your temporary sanctuary, and your body betrays you with relentless urgency. You’re not alone. Millions of people worldwide grapple with the debilitating symptoms of ulcerative colitis, a chronic inflammatory bowel disease that affects the colon. This relentless disease can disrupt your daily life, leaving you feeling drained and uncertain. But there is hope. A well-structured nursing care plan can empower you to navigate the challenges of ulcerative colitis and regain control of your health. This article serves as your guide, offering comprehensive information and actionable steps to manage this disease effectively.
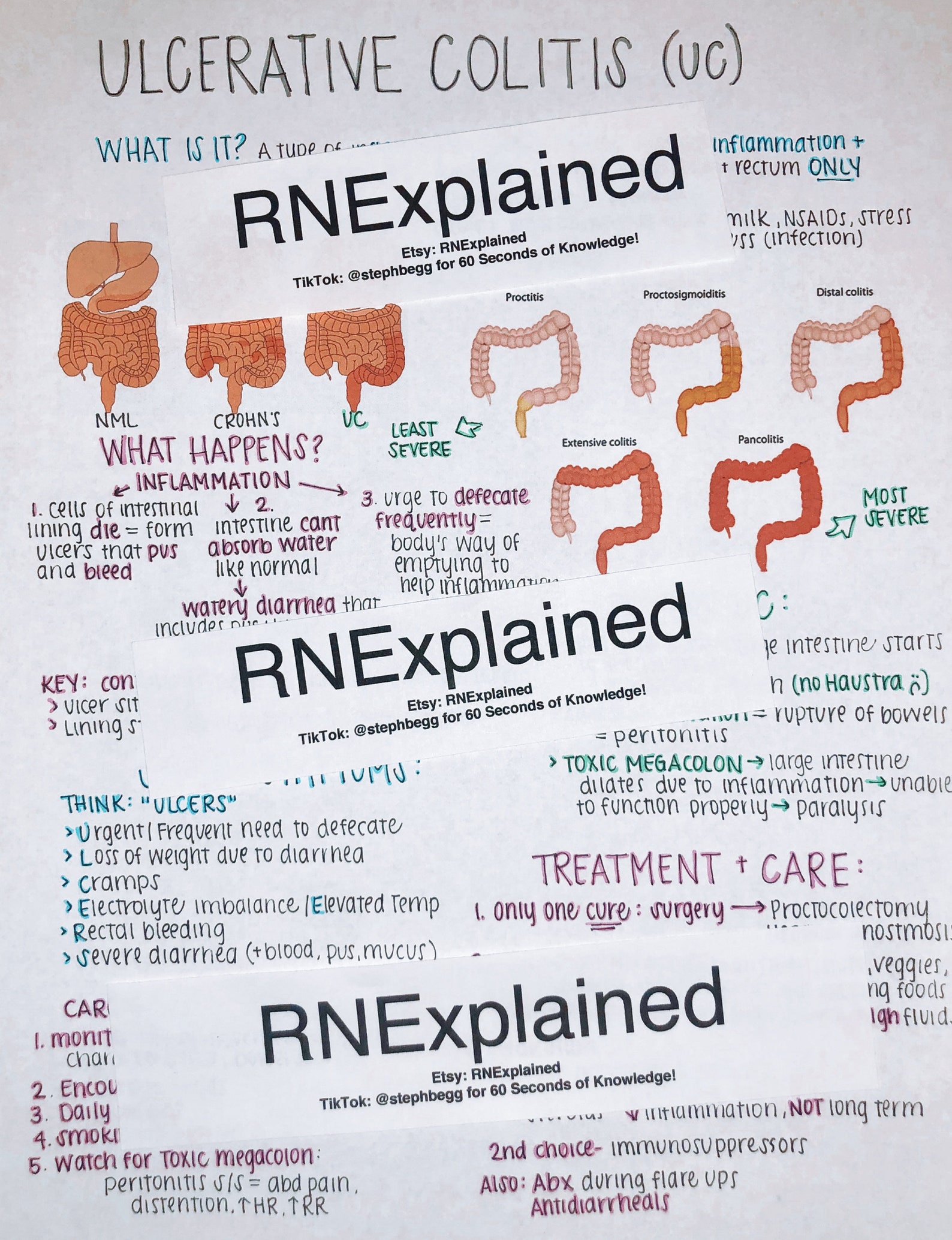
Image: www.etsy.com
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) that causes inflammation and ulcers in the lining of the colon, the large intestine. It can lead to symptoms like diarrhea, abdominal pain, rectal bleeding, and weight loss. While there’s no cure for ulcerative colitis, effective nursing care plans can help manage symptoms, minimize complications, and improve your overall quality of life.
Understanding the Foundation: A Nursing Care Plan for Ulcerative Colitis
A holistic nursing care plan for ulcerative colitis isn’t just about managing symptoms; it’s about empowering individuals to actively participate in their own care. It includes a comprehensive assessment of the patient’s needs, development of individualized goals, and implementation of tailored interventions. The nursing care plan acts as a roadmap to navigate the complexities of this disease while promoting overall well-being.
Assessment: The Cornerstone of Personalized Care
Before embarking on the journey to manage ulcerative colitis, it’s crucial to understand the individual’s needs. A thorough assessment serves as the foundation upon which the nursing care plan is built.
- Gathering Information: The nurse will gather information about the patient’s medical history, current symptoms, medications, lifestyle, and emotional well-being.
- Physical Examination: The physical examination assesses vital signs, observing signs of dehydration, nutritional deficiencies, and complications.
- Diagnostic Tests: Depending on the situation, the nurse may need to facilitate the ordering of diagnostic tests like colonoscopy, blood work, and stool studies to confirm diagnosis or monitor disease activity.
- Psychological Assessment: The mental and emotional impact of chronic illness is often overlooked. The nurse assesses the patient’s coping mechanisms, social support systems, and anxiety levels related to the disease.
Setting Goals: Defining Success Together
With the assessment complete, the focus shifts to setting clear, achievable goals. Recognizing the patient’s individual needs and aspirations is vital.
- Symptom Management: The primary goal is reducing the frequency and severity of symptoms like diarrhea, abdominal pain, and rectal bleeding.
- Nutritional Optimization: Ensuring adequate nutrition is critical for maintaining strength and energy levels. The nurse may work with a registered dietitian to create a personalized dietary plan.
- Medication Compliance: Understanding the various medications used to treat ulcerative colitis, including their side effects and proper administration, is essential for successful management.
- Emotional Support: The nurse helps the patient access resources and strategies to manage stress and maintain a positive outlook.
- Disease Education: Patients need to be empowered with knowledge about their condition. The nurse provides information about trigger factors, self-management techniques, and available resources.

Image: www.pinterest.com
Implementing Interventions: Putting the Plan into Action
The nursing care plan is a living document that adapts to the patient’s ever-changing needs. Interventions are implemented based on the ongoing assessment and goal setting.
- Medication Administration: Administering prescribed medications, including anti-inflammatory drugs, immunosuppressants, and biologics, according to the doctor’s orders.
- Fluid and Electrolyte Management: Maintaining adequate hydration is critical, especially for individuals experiencing diarrhea. The nurse assists patients in identifying appropriate fluid intake strategies.
- Nutritional Counseling: Collaborate with a registered dietitian to develop a balanced diet that minimizes digestive discomfort and supports overall health.
- Wound Care: In cases of rectal bleeding or perianal ulcers, the nurse provides wound care and education on proper hygiene to prevent infections.
- Bowel Training: Regular bowel habits are essential for managing ulcerative colitis. The nurse assists in developing a bowel training program, including dietary adjustments and timed bathroom visits.
- Stress Reduction Techniques: Stress can trigger flares. The nurse teaches relaxation techniques, mindfulness, and other stress reduction strategies.
- Psychosocial Support: Connect patients with support groups, mental health professionals, or other resources to address emotional and psychological needs.
- Monitoring and Evaluation: Regular monitoring is crucial to assess the effectiveness of the nursing care plan, identify any emerging issues, and make necessary adjustments.
Expert Insights and Actionable Tips
Navigating the complexities of ulcerative colitis can feel daunting, but remember that you are not alone. Seeking support from healthcare professionals and embracing the right tools can significantly empower you in your journey.
- Communicate Openly with your Healthcare Team: Engaging in open and honest communication with your healthcare provider is vital. Sharing your concerns, frustrations, and even successes will help them tailor your care plan to your specific needs.
- Maintain a Symptom Diary: Keep track of your symptoms, including frequency, severity, and any potential triggers. This data can provide invaluable insights for your healthcare team, aiding in adjusting medications and managing flare-ups.
- Embrace a Balanced Diet: Food plays a crucial role in managing ulcerative colitis. Avoid known trigger foods and focus on a balanced diet that includes plenty of fruits, vegetables, and whole grains. Consult with a registered dietitian for personalized dietary guidance.
- Explore Complementary Therapies: Complementary therapies like yoga, meditation, and acupuncture can complement conventional treatment by reducing stress and promoting overall well-being.
- Join a Support Group: Connecting with others who understand what you’re going through can provide immense support and encouragement. Seek out local or online support groups for individuals living with ulcerative colitis.
Nursing Care Plan For Ulcerative Colitis
Conclusion: Embracing a Lifestyle of Empowerment
Living with ulcerative colitis presents unique challenges, but with the right care plan, you can manage your symptoms, prevent complications, and embrace a fulfilling life. Remember, you are not alone. Seek support from your healthcare team, engage in open communication, and empower yourself with knowledge about your condition. By actively participating in your care, you can navigate the complexities of this disease and reclaim control of your health.
Note: This article provides general information. It is not a substitute for professional medical advice or treatment. Always consult with your healthcare provider for personalized guidance and care.






