The first time I saw a child with a cleft lip and palate, I was overwhelmed with a mixture of emotions: sadness for the child, curiosity about the condition, and a deep desire to understand how I could help. As a nurse, I knew that caring for children with cleft lip and palate would require a specific understanding of their needs and challenges. This journey led me to delve into the world of nursing diagnoses for this condition, and I discovered a profound impact these diagnoses have on providing holistic care.
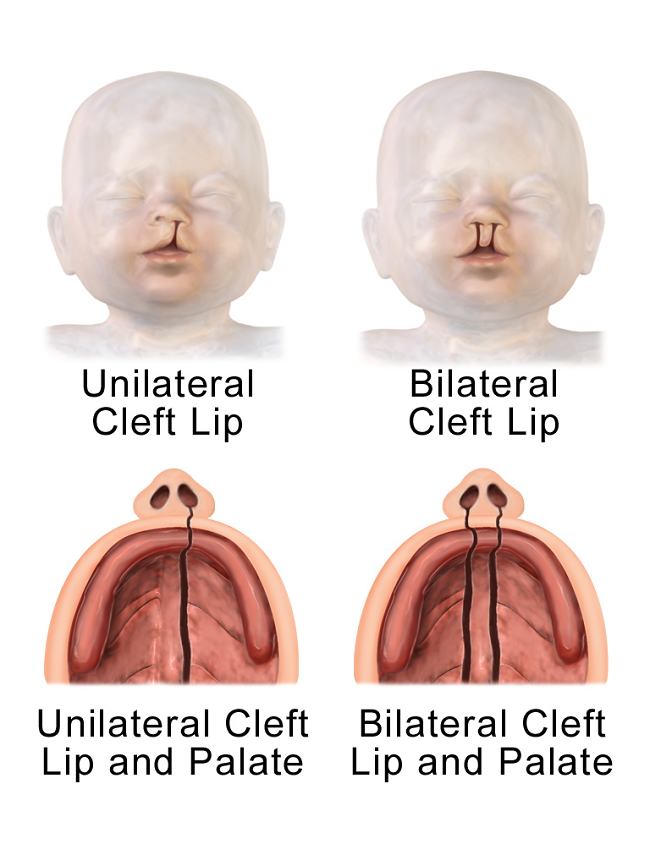
Image: www.alomedika.com
Understanding the complexities of cleft lip and palate beyond the physical appearance is crucial. It’s not just about the way the child looks; it’s about the impact on their feeding, breathing, speech, and social development. This intricate understanding is where nursing diagnoses come into play, acting as a compass to guide nursing interventions and ensure the best possible outcomes for these children and their families.
Understanding Cleft Lip and Palate: The Basics
Cleft lip and palate are congenital birth defects that occur when the upper lip and/or roof of the mouth don’t close completely during pregnancy. These conditions can range in severity, from a small notch in the lip to a complete opening in both the lip and palate.
Cleft lip is a split or opening in the upper lip, which can affect one or both sides. Cleft palate occurs when the roof of the mouth doesn’t close completely, leaving an opening that can range from small to large and can extend to the back of the throat. When both the lip and the palate are affected, it’s called a cleft lip and palate.
Common Nursing Diagnoses for Cleft Lip and Palate
Nursing diagnoses are clinical judgments about an individual’s response to actual or potential health problems. They provide a framework for identifying patient needs and developing individualized care plans. Here are some of the most common nursing diagnoses for children with cleft lip and palate:
1. Impaired Oral Mucous Membrane Related to Surgical Intervention
This diagnosis reflects the potential for the oral mucous membrane to become damaged following surgery. The delicate tissues in the mouth, especially after surgical repair, are susceptible to injury from feeding, suctioning, or other procedures. The nurse plays a crucial role in identifying potential problems and implementing interventions to protect the oral mucosa.

Image: www.coursehero.com
2. Risk for Impaired Skin Integrity Related to Frequent Feeding Practices
Children with cleft lip and palate may require specialized feeding techniques and devices that can irritate the delicate skin around the mouth. This diagnosis indicates the risk for skin breakdown, particularly in areas where the feeding tube or other equipment comes into contact with the skin. Nurses need to monitor the skin’s condition frequently and implement measures like skin protection and barrier creams to prevent irritation.
3. Risk for Aspiration Related to Impaired Swallowing
The structural abnormalities associated with cleft lip and palate can affect the child’s ability to swallow safely. This diagnosis highlights the risk of aspiration, meaning that food or liquids could enter the airways instead of the stomach. Nurses are vital in identifying signs of aspiration and using interventions like positioning techniques, feeding schedules, and specialized feeding techniques to minimize the risk.
4. Risk for Delayed Growth and Development Related to Inefficient Feeding and Nutrient Intake
Children with cleft lip and palate can experience difficulties feeding, which can lead to inadequate nutrition and subsequent delays in growth and development. Nurses play a critical part in assessing the child’s nutritional status, monitoring growth patterns, and collaborating with other healthcare professionals to ensure adequate nutrition and support optimal development.
5. Impaired Family Coping Related to the Diagnosis of Cleft Lip and Palate
Receiving a diagnosis of a serious birth defect like cleft lip and palate can be overwhelming for families. This diagnosis recognizes the emotional, financial, and practical stressors families face. Nurses can support families by providing emotional support, information about resources, and guidance to help them cope with the challenges of caring for a child with a cleft.
Latest Trends and Developments
The field of cleft lip and palate care is constantly evolving. One significant trend is the increasing emphasis on multidisciplinary care teams, where pediatricians, nurses, surgeons, speech therapists, and other specialists work together from the initial diagnosis through ongoing treatment and support. This collaborative approach ensures that each child’s complex needs are addressed holistically.
Another significant development is the rise of telehealth, which allows healthcare professionals to provide remote consultations and support for children with cleft lip and palate. This is particularly beneficial in rural areas or where access to specialized care is limited.
Tips and Expert Advice
Providing care for a child with cleft lip and palate requires specialized knowledge and understanding. Here are some tips from my experience as a nurse specializing in this area:
- Educate yourself about cleft lip and palate. The more you know about the condition, the better equipped you will be to provide compassionate and effective care.
- Maintain open communication with the family and child. Listen to their concerns and address their questions and needs.
- Collaborate with other healthcare professionals. A multidisciplinary approach ensures comprehensive care for the child.
- Promote bonding and attachment between the family and child. Encourage skin-to-skin contact and provide opportunities for nurturing interactions.
- Advocate for the child’s needs. Ensure the child receives appropriate care and support in all aspects of their life.
Empathy and understanding are essential. Remember that even the smallest act of kindness or compassion can make a big difference in the life of a child with cleft lip and palate and their family. By providing knowledgeable, supportive, and patient-centered care, nurses play a crucial role in improving the quality of life for these children.
FAQs About Nursing Diagnosis for Cleft Lip and Palate
Q: How are nursing diagnoses used in patient care?
A: Nursing diagnoses provide a common language and framework for nurses to communicate about patients’ needs and plan care. They help nurses identify problems, develop interventions, and evaluate the effectiveness of care.
Q: What are the key interventions for children with cleft lip and palate?
A: Interventions depend on the specific needs of the child but may include specialized feeding techniques, safe feeding positioning, oral hygiene instructions, speech therapy, surgical interventions, and psychosocial support for the family.
Q: Where can I find more information about cleft lip and palate?
A: There are many resources available, including websites like the American Cleft Palate-Craniofacial Association (ACPA) and the National Cleft Palate Foundation (NCPF). You can also find support groups and online communities for families affected by these conditions.
Nursing Diagnosis For Cleft Lip And Palate
Conclusion
Nursing diagnoses are essential tools in providing comprehensive, holistic care for children with cleft lip and palate. By understanding the unique needs and challenges these children and their families face, nurses can develop targeted interventions and provide support throughout the treatment and recovery process.
Are you interested in learning more about caring for children with cleft lip and palate? Share your thoughts in the comments below!






