Imagine a mother-to-be, preparing for the joyous arrival of her baby. Suddenly, a wave of panic washes over her – she feels a strange sensation, a sense of urgency, and a terrifying fear for her unborn child. This is the reality of an umbilical cord prolapse, a life-threatening emergency that requires immediate attention and swift action. For nurses, understanding how to identify, diagnose, and manage this condition is crucial in ensuring the well-being of both mother and baby.
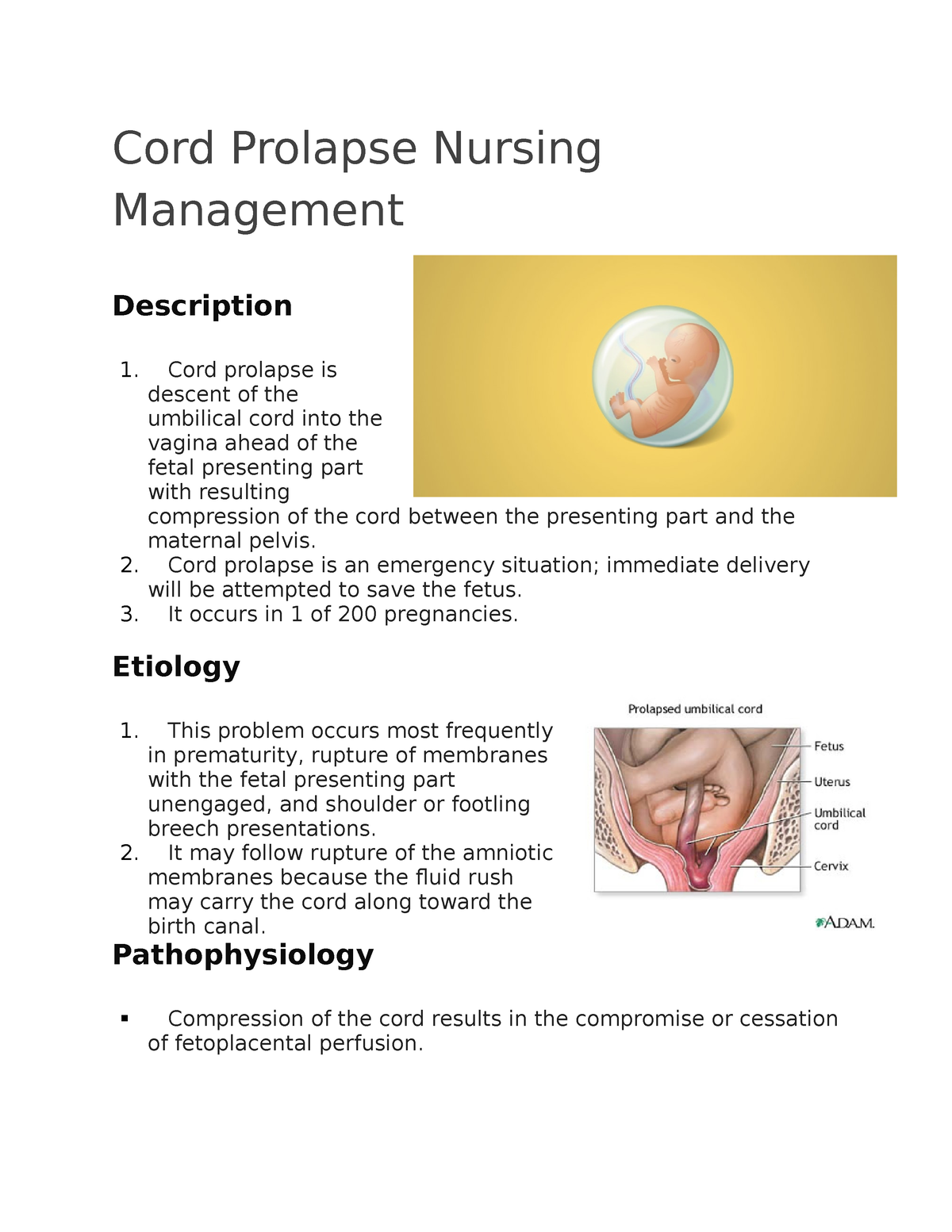
Image: www.studocu.com
Umbilical cord prolapse occurs when the umbilical cord descends through the cervix into the vagina before the presenting part of the fetus, putting the baby at risk of oxygen deprivation. Understanding the intricacies of this condition, including its underlying causes, associated risks, and the crucial role of nursing diagnosis, is essential for nurses to provide optimal care during labor and delivery.
Defining the Problem: Understanding Umbilical Cord Prolapse
The umbilical cord is a lifeline for the fetus, carrying nourishment and oxygen through the veins and arteries. When it slips down before the baby’s head, it can become compressed against the baby’s head or the cervix, disrupting blood flow to the placenta and potentially causing fetal distress.
To grasp the gravity of this situation, it’s vital to understand the typical progression of labor. The baby’s presenting part—usually the head—acts as a buffer, blocking the cord from prolapsing. However, when the presenting part isn’t fully engaged or when there is a breech presentation, the cord can descend. This can occur during labor or even during a premature rupture of membranes.
Recognizing the Signs: Crucial Clues for Identifying Umbilical Cord Prolapse
Early detection is crucial in preventing severe complications. Nurses play a vital role in recognizing the telltale signs of this emergency. While some signs are obvious, others might be subtle. Recognizing the following signs can be a lifesaver:
Visible Signs:
- Palpable cord: Nurses might physically feel the cord in the vaginal canal during a vaginal examination.
- Visible cord: The cord can sometimes be seen protruding through the cervical opening. This is a clear and alarming sign.

Image: www.coursehero.com
Signs of Fetal Distress:
- Fetal bradycardia: A significantly slow fetal heart rate could indicate oxygen deprivation due to cord compression.
- Variable decelerations: Variable decelerations on the fetal heart rate monitor are common with cord compression and may be sharp, deep, and unpredictable.
- Loss of fetal heart rate variability: The normal variability in fetal heart rate may become absent, suggesting a serious lack of oxygen.
The Critical Role of Nursing Diagnosis: Guiding the Emergency Response
Once the signs of cord prolapse are recognized, the nursing diagnosis becomes pivotal in initiating prompt and effective interventions. The most common nursing diagnosis associated with umbilical cord prolapse is “Risk for Impaired Fetal Gas Exchange.” This diagnosis clearly outlines the immediate threat to the fetus and guides nursing actions.
Other nursing diagnoses may also be relevant depending on the individual patient’s situation. For instance, “Anxiety” or “Fear” might be appropriate for the mother experiencing distress and uncertainty. “Deficient Knowledge” about the condition could also be applied to educate the mother and her partner about the situation and potential complications.
Nursing Interventions: Restoring Blood Flow and Ensuring Safety
Nursing interventions are crucial in addressing the immediate threat of cord compression and ensuring the safety of both mother and baby. These interventions must be swift, decisive, and coordinated with the medical team.
Immediate Actions:
- Relieve pressure on the cord: The nurse should immediately elevate the presenting part of the fetus by using a hand to gently lift the baby’s head or breech away from the cord. This prevents further compression and allows blood flow to the baby.
- Position the mother: The mother should be positioned in a knee-chest or Trendelenburg position. This maneuver positions the uterus higher than the baby’s head, helping to relieve the pressure on the cord.
- Administer oxygen: Oxygen administered to the mother can help increase the oxygen supply to the fetus and compensate for the reduced blood flow.
- Monitor fetal heart rate: Constant monitoring of the fetal heart rate is essential to assess the effectiveness of the interventions and identify any changes in fetal condition.
- Administer medications: Medications may be prescribed to accelerate the baby’s delivery, such as a tocolytic agent to temporarily stop labor contractions.
Continuous Monitoring:
The nurse’s role doesn’t end after the initial interventions. Continuous monitoring of the mother and baby is vital, including:
- Fetal heart rate monitoring: The fetal heart rate should be monitored continuously, looking for changes and signs of distress.
- Maternal vital signs: The mother’s blood pressure, pulse, and respiratory rate should be monitored closely for any signs of instability.
- Vaginal examinations: Periodic vaginal examinations might be necessary to assess the cord’s position and the baby’s descent.
- Emotional support: Nurses provide emotional support to the mother and her partner, who are likely to be experiencing anxiety and fear during this stressful situation.
The Path to Recovery: Addressing Long-Term Concerns
Once the immediate crisis is managed, the focus shifts towards supporting the mother and baby through the delivery process. A cesarean delivery is often the safest and most effective way to deliver the baby in cases of umbilical cord prolapse, ensuring the least amount of risk for both mother and baby.
The recovery process for the baby may involve monitoring for signs of oxygen deprivation, including seizures, brain hemorrhage, or respiratory distress. Depending on the severity of the compromise, the baby might require intensive care and specialized support.
Nurses continue to play a crucial role in monitoring the baby’s recovery, providing education to the parents, and encouraging a safe and stable environment for bonding and breastfeeding. They also help coordinate the baby’s post-discharge follow-up care with specialists like a neonatologist or pediatrician.
Preventative Measures: Understanding the Roots of the Problem
While not always preventable, understanding the underlying causes of cord prolapse can inform preventative measures. Here’s a breakdown of common contributing factors:
Factors Contributing to Cord Prolapse:
- Premature rupture of membranes: This can occur before the baby’s head is engaged in the pelvis, leaving space for the cord to descend.
- Polyhydramnios: Excessive amniotic fluid can create a larger space for the cord to prolapse.
- Short umbilical cord: A short umbilical cord makes it more susceptible to prolapse as the baby descends.
- Breech presentation: When the baby’s buttocks or feet present first, it removes the barrier against the cord descending.
- Multiple gestation: With twins or more, the space for the cord becomes narrower, increasing the risk of prolapse.
- Previous cord prolapse: This can be a risk factor for future pregnancies.
Nursing Diagnosis For Umbilical Cord Prolapse
Nurses: The Guardians of Safety
Understanding the complexities of umbilical cord prolapse is essential for nurses working in labor and delivery units. They play a vital role in identifying the warning signs, initiating prompt interventions, and supporting the mother and baby through this critical period.
By staying informed about the latest advancements, adhering to established protocols, and demonstrating unwavering dedication to patient safety, nurses contribute significantly to positive outcomes and ensure the well-being of both mother and child. As dedicated healthcare professionals, nurses are the guardians of safety, guiding families through challenging moments and ensuring a brighter future for new life.






