Imagine waking up feeling tired and unmotivated, the thought of food just not appealing. You’re not alone. Poor appetite, also known as anorexia, is a common concern that can stem from various factors and significantly impact an individual’s health and well-being. This is where a comprehensive nursing care plan steps in, offering a roadmap to restoring and maintaining optimal nutritional health.
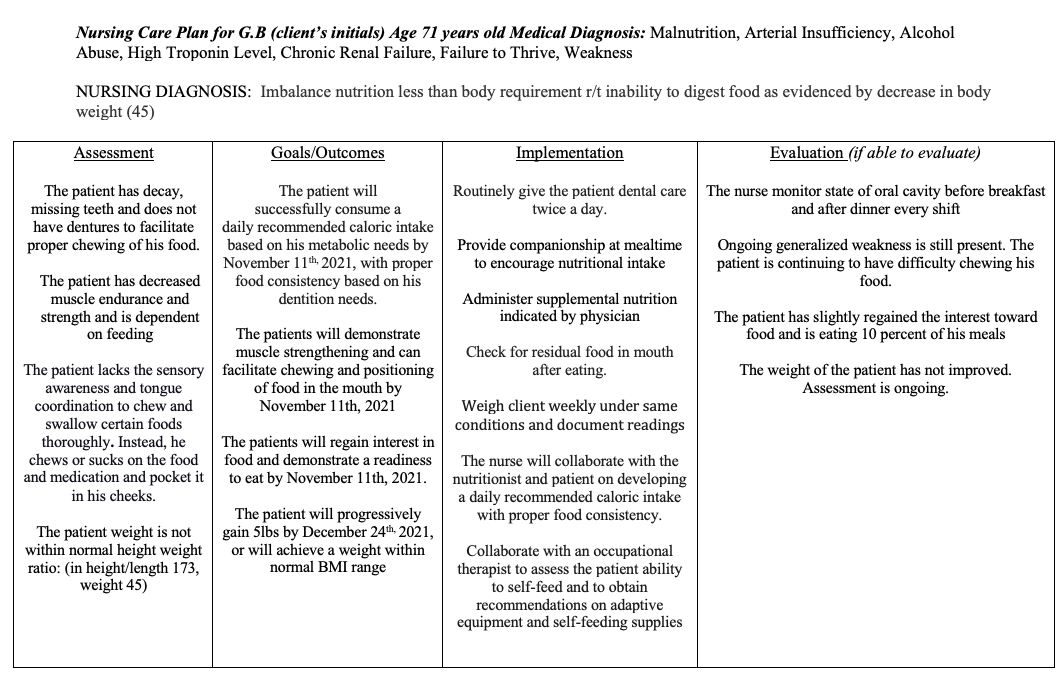
Image: www.chegg.com
A nursing care plan for poor appetite is a personalized blueprint designed to address the underlying causes of diminished food intake, promote a healthy relationship with eating, and ultimately enhance the patient’s overall well-being. This plan is tailored to each individual’s unique needs and may involve a combination of medical, nutritional, and psychological interventions, all carefully coordinated by a skilled and compassionate nursing team.
Understanding the Root Cause
Medical Evaluation
The journey to resolving poor appetite begins with a thorough medical evaluation. It is crucial to identify any underlying medical conditions that may be contributing to the lack of appetite, such as:
- Gastrointestinal disorders: Conditions like gastritis, ulcers, or irritable bowel syndrome can impede food intake due to discomfort or digestive issues.
- Metabolic conditions: Diabetes, thyroid disorders, and even kidney disease can significantly affect appetite and energy levels.
- Infections: Viral or bacterial infections, particularly those affecting the respiratory system, often cause a loss of taste and smell, impacting appetite.
- Cancer: Certain types of cancer and their treatments, such as chemotherapy, can lead to nausea, vomiting, and a diminished appetite.
- Neurological conditions: Parkinson’s disease, dementia, and stroke can disrupt the brain’s signals controlling appetite and swallowing.
Psychological and Social Factors
Beyond medical conditions, certain psychological and social factors can also play a role in poor appetite. These include:
- Depression and anxiety: Mental health issues often manifest as a lack of motivation and interest in food, leading to poor dietary habits.
- Grief and stress: Life events like bereavement or significant stress can affect eating patterns and contribute to a decrease in appetite.
- Social isolation: Loneliness and lack of social interaction can lead to a diminished sense of enjoyment in mealtimes, impacting appetite.
- Food insecurity: Limited access to food, financial constraints, and lack of resources can contribute to poor nutrition and inadequate intake.
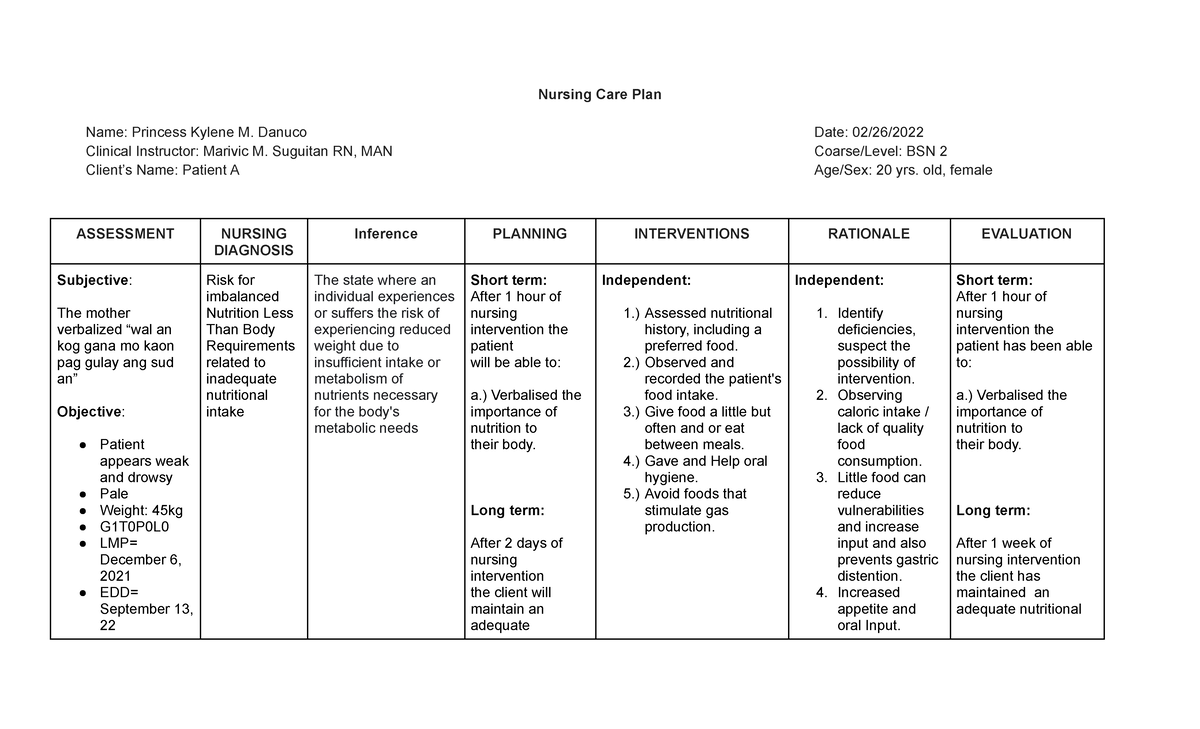
Image: www.studocu.com
Developing a Personalized Nursing Care Plan
Once the root cause of poor appetite is identified, a tailored nursing care plan is developed to address the specific needs of each patient. This might involve a combination of these strategies:
Nutritional Interventions
The core of a nursing care plan focuses on optimizing the patient’s nutritional intake. This involves:
- Dietary modifications: A registered dietitian can create a personalized meal plan considering the patient’s individual needs and preferences. This might involve increasing calorie density, incorporating nutrient-rich foods, or adjusting meal frequency and portion sizes.
- Meal enrichment: Adding fortified foods or supplements to ensure adequate nutrient intake, particularly when dietary restrictions are in place.
- Oral hygiene: Maintaining good oral hygiene can enhance taste and smell, improving appetite. This involves regular brushing, flossing, and addressing any dental problems.
- Liquid intake: Staying hydrated is crucial for overall well-being and can help maintain appetite. Ensure patients consume adequate fluids, especially during illness or recovery.
Medications and Treatments
In certain cases, medications may be necessary to address the underlying medical condition contributing to poor appetite. For example,:
- Anti-nausea medications: These can relieve nausea and vomiting, improving appetite and reducing food aversion.
- Anti-depressants: Addressing underlying depression can improve motivation and interest in food.
- Appetite stimulants: In some cases, medications like megestrol acetate or dronabinol may be prescribed to stimulate appetite and increase food intake.
Psychological Support
Addressing the psychological aspects of poor appetite is crucial for long-term success. This can involve:
- Cognitive behavioral therapy (CBT): Cognitive behavioral therapy can help patients identify and challenge negative thoughts and behaviors related to food and eating.
- Stress management techniques: Relaxation techniques, meditation, and mindfulness exercises can help reduce stress and improve appetite.
- Social support: Encourage patients to connect with loved ones and participate in social activities to foster a sense of well-being and enjoyment in mealtimes.
Environmental Modifications
Making adjustments to the patient’s environment can also contribute to improved appetite:
- Pleasant mealtime atmosphere: Create a calm, relaxing environment for meals. This can involve soft music, comfortable seating, and pleasant lighting.
- Social interaction: Encourage the patient to eat with others, promoting companionship and enjoyment of meals.
- Avoid distractions: Minimize distractions during mealtimes, such as television or work, to focus on the experience of eating.
Monitoring and Evaluation
The nursing care plan is a dynamic process, continuously evaluated and adjusted based on the patient’s progress and response to treatment. This involves:
- Regular weight monitoring: Track weight changes to assess the effectiveness of the care plan.
- Dietary intake assessment: Monitor food intake to identify patterns and areas for improvement.
- Monitoring for signs of malnutrition: Observe for signs of deficiencies or malnutrition, adjusting the care plan as needed.
The Role of Nurses in Promoting Appetite
Nurses play a pivotal role in the success of a nursing care plan for poor appetite. They provide empathetic care, assess the patient’s needs, administer medications effectively, and educate patients and families about the plan’s key components.
Moreover, nurses foster a positive and supportive environment, encouraging the patient to engage in healthy eating habits without judgment or pressure. By collaborating with other healthcare professionals, such as dietitians, physicians, and therapists, nurses ensure a holistic approach to addressing the multifaceted nature of poor appetite.
Nursing Care Plan For Poor Appetite
Conclusion
A nursing care plan for poor appetite is a critical component of restoring and maintaining nutritional well-being. By addressing the underlying causes, adopting personalized strategies, and providing ongoing support, nurses empower patients to regain their appetite and thrive. This comprehensive approach involves a collaborative effort between healthcare professionals and the patient, ultimately leading to a brighter and healthier future. Remember, if you or a loved one is struggling with poor appetite, seeking professional guidance is a crucial step in regaining your nutritional health and well-being.






