Imagine a scenario where your hands feel numb and cold, even on a warm day. You struggle to feel the warmth of a cup of hot cocoa, your fingertips tingle incessantly, and your extremities appear pale and discolored. This is a glimpse into the uncomfortable reality of ineffective peripheral tissue perfusion. This condition, characterized by inadequate blood flow to the extremities, can be a frustrating and sometimes alarming experience, warranting a comprehensive care plan to restore proper circulation and alleviate associated symptoms.

Image: www.scribd.com
Understanding the intricacies of ineffective peripheral tissue perfusion is paramount for developing an effective care plan. This article dives into the mechanisms behind this condition, its varied causes, and the multi-faceted approach required for its management. We’ll explore the importance of lifestyle modifications, pharmacotherapy, and advanced interventions to improve blood flow and enhance the overall well-being of individuals experiencing suboptimal tissue perfusion.
Dissecting Ineffective Peripheral Tissue Perfusion: Unveiling the Mechanisms
Delving into the Fundamentals
Before delving into the intricacies of care plans, it’s crucial to understand the fundamentals of peripheral tissue perfusion. Essentially, this refers to the efficient delivery of oxygenated blood to tissues located in the extremities, such as the hands, feet, and legs. This process relies on a delicate dance between the heart, arteries, veins, and the intricate network of capillaries that permeate our tissues.
The Complex Web of Circulation
The heart acts as the powerhouse of this circulation, pumping oxygen-rich blood through arteries that branch out like a tree, reaching the furthest points of our limbs. As blood travels to these distant locations, it releases vital oxygen and nutrients to the cells. The spent blood, now oxygen-deprived, embarks on a return journey through veins, ultimately flowing back to the heart to be replenished with oxygen before venturing out again.
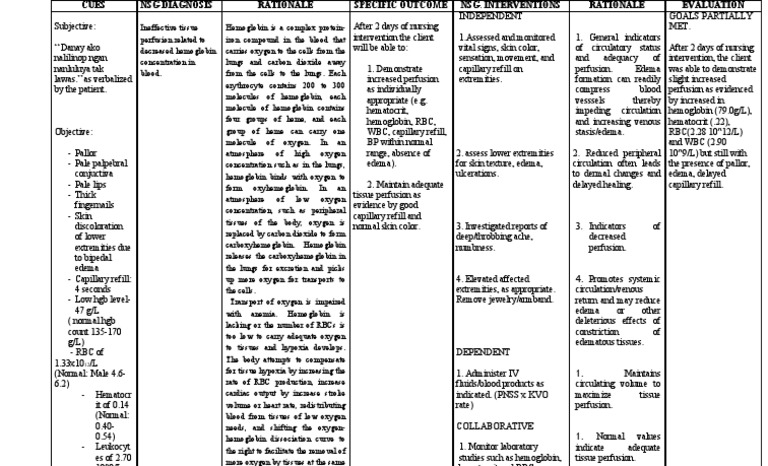
Image: www.scribd.com
When the Flow Stalls: The Genesis of Ineffective Perfusion
Ineffective peripheral tissue perfusion arises when this intricate circulatory rhythm becomes disrupted. A variety of factors can impede blood flow, causing a reduction in the delivery of oxygen and nutrients to the extremities. This can result in a cascade of symptoms, ranging from mild discomfort to potentially severe complications.
The Spectrum of Causes: Unraveling the Roots of Ineffective Perfusion
The causes of ineffective peripheral tissue perfusion span a broad spectrum, ranging from Lifestyle choices to underlying medical conditions. Understanding these contributing factors is essential for tailoring an effective care plan.
Lifestyle Factors: The Pillars of Prevention
Many lifestyle choices can significantly influence peripheral tissue perfusion. Some key contributors include:
- Smoking: Nicotine, a primary component of cigarettes, constricts blood vessels, hindering blood flow to the extremities, particularly in individuals with existing circulatory conditions.
- Sedentary Lifestyle: Lack of physical activity leads to weakened muscles, including those in the legs, which can impair venous return and contribute to inadequate blood flow to the lower extremities.
- Obesity: Excess body weight can place a strain on the heart and circulatory system, making it harder for the body to effectively pump blood to the peripheral tissues.
- Diet: A diet high in saturated fats and cholesterol can contribute to the development of atherosclerosis, a condition characterized by plaque buildup in blood vessels, narrowing the passage for blood flow.
- Excessive Alcohol Consumption: Excessive alcohol intake can damage blood vessels, leading to impaired circulation.
Medical Conditions: A Deeper Dive
Beyond lifestyle choices, certain medical conditions can contribute to or directly cause ineffective peripheral tissue perfusion. Some notable examples include:
- Peripheral Artery Disease (PAD): PAD is a common condition that afflicts blood vessels in the legs and feet, often stemming from atherosclerosis. This condition can obstruct blood flow, leading to pain, cramping, and intermittent claudication.
- Diabetes: Diabetes can damage blood vessels, making them more susceptible to narrowing and blockage, leading to poor circulation to the extremities.
- Raynaud’s Phenomenon: This condition involves spasms in the blood vessels of the fingers and toes, triggered by cold temperatures or stress, leading to temporary restriction of blood flow and color changes in the affected extremities.
- Deep Vein Thrombosis (DVT): DVT is a condition where blood clots form within the deep veins, most commonly in the legs. These clots can obstruct blood flow, leading to pain, swelling, and discoloration of the affected leg.
- Heart Failure: The weakened pumping action of the heart in heart failure can diminish blood flow to the extremities, resulting in reduced tissue perfusion.
- Aortic Aneurysm: An aortic aneurysm, a bulging or weakening of the aorta, can disrupt blood flow to the legs and feet if it affects the descending aorta.
Navigating the Care Plan: From Diagnosis to Management
A comprehensive care plan for ineffective peripheral tissue perfusion should be tailored to the individual’s specific needs, considering the underlying cause, symptoms, and overall health status. It’s essential to collaborate closely with healthcare professionals to develop an approach that addresses the unique challenges faced by each patient.
Diagnosis: Unraveling the Root Cause
The first step in managing ineffective peripheral tissue perfusion is establishing a definitive diagnosis. A thorough medical history, physical examination, and a battery of diagnostic tests are often employed to determine the underlying cause. Key diagnostic tools include:
- Ankle-Brachial Index (ABI): This non-invasive test measures blood pressure in the ankles and compares it to the blood pressure in the arms, providing insights into the degree of blood flow restriction in the legs.
- Doppler Ultrasound: This imaging technique uses sound waves to evaluate blood flow in arteries and veins, identifying blockages, narrowing, or other abnormalities in blood vessels.
- Angiography: This invasive procedure involves injecting a contrast dye into the blood vessels, allowing visualization of the arteries on X-ray, revealing blockages or narrowing.
Management: A Multifaceted Approach
Once the underlying cause is identified, the care plan for ineffective peripheral tissue perfusion will focus on addressing the specific contributing factors and improving blood flow to the extremities.
Lifestyle Modifications: The Foundation of Long-Term Well-being
Lifestyle changes are often the cornerstone of managing ineffective peripheral tissue perfusion. These modifications aim to optimize blood flow and minimize the risk of complications. Key lifestyle recommendations include:
- Smoking Cessation: Quitting smoking is essential for improving blood flow and reducing the risk of cardiovascular disease.
- Regular Exercise: Engaging in regular physical activity helps to improve blood circulation and strengthen leg muscles, promoting effective venous return.
- Dietary Changes: Adopting a heart-healthy diet low in saturated fats and cholesterol, rich in fruits, vegetables, and whole grains, can improve blood flow and prevent further damage to blood vessels.
- Weight Loss: If you are overweight or obese, losing weight can significantly reduce the strain on your heart and circulatory system, improving blood flow to the extremities.
- Avoid Cold Exposure: Individuals with Raynaud’s phenomenon should avoid exposure to cold temperatures, as this can trigger spasms in blood vessels, leading to reduced blood flow. Warm clothing and gloves are essential for staying warm in cold weather.
Pharmacotherapy: Medications to Enhance Circulation
In some cases, medication is necessary to improve blood flow and alleviate symptoms. Commonly prescribed medications for ineffective peripheral tissue perfusion include:
- Antiplatelet Medications: Aspirin and clopidogrel are examples of antiplatelet medications that prevent blood clots from forming, reducing the risk of blockages in blood vessels.
- Statins: These medications lower cholesterol levels, reducing the buildup of plaque in blood vessels and promoting better blood flow.
- Calcium Channel Blockers: These medications relax blood vessels, improving blood flow by widening the passage for blood.
- Vasodilators: This class of medications dilates blood vessels, directly enhancing blood flow to the extremities.
Advanced Interventions: Restoring Blood Flow
For severe cases of ineffective peripheral tissue perfusion or when lifestyle modifications and medications are insufficient, specialized medical interventions may be necessary to restore blood flow and alleviate symptoms. Common interventions include:
- Angioplasty: This minimally invasive procedure uses a balloon catheter to open a blocked or narrowed artery, restoring blood flow.
- Stenting: After angioplasty, a tiny wire mesh tube called a stent is often placed in the artery to keep it open and prevent it from narrowing again.
- Bypass Surgery: In some cases, particularly for severe PAD, bypass surgery may be required. This procedure involves grafting a healthy segment of blood vessel from another part of the body to bypass the blocked or narrowed artery, restoring blood flow to the affected limb.
Embracing a Holistic Approach: A Path Towards Wellness
Managing ineffective peripheral tissue perfusion requires a holistic approach that incorporates lifestyle modifications, medication, and when necessary, advanced interventions. Close collaboration with healthcare professionals, including vascular specialists, is essential for developing a tailored care plan that addresses the individual’s specific needs. This collaborative approach allows for continuous monitoring, adjustments to the care plan based on individual response, and early intervention to prevent complications.
Care Plan For Ineffective Peripheral Tissue Perfusion
Conclusion: Empowering Yourself with Knowledge
Ineffective peripheral tissue perfusion can pose a significant challenge to one’s quality of life. However, by understanding the underlying mechanisms, identifying the contributing factors, and embracing a comprehensive care plan, individuals can take control of their health and work towards restoring optimal blood flow to their extremities. This article serves as a valuable starting point, sparking conversations with healthcare professionals and empowering individuals to seek appropriate medical guidance and manage their condition effectively.






